Light Therapy: Selectively Targeting Liver Cancer Cells

By Paul Brockwell Jr., MCV Foundation
This is the stuff of sci-fi dreams: healing cancer patients through focused light beams. While the idea sounds light-years away, it could soon become a reality thanks to the work of researchers here on the MCV Campus.
Seung Duk Lee, M.D., Ph.D., associate surgical director of liver transplants for the VCU Health Hume-Lee Transplant Center, has been researching potential therapies using targeted light to selectively kill hepatocellular carcinoma (HCC).
VCU is unique. We have research staff and clinical staff working hand in hand. Because of that, we’re able to do advanced research that maybe other centers aren’t able to.
Kush Savsani, a first-year medical student
HCC is the most common type of liver cancer and the third leading cause of cancer-related deaths. In 2024, the American Cancer Society estimated more than 41,630 new cases will be diagnosed in the U.S., with 29,840 deaths. Treatment can be challenging depending on the size and location of the tumor cells, as well as a patient’s overall health. It also is most prevalent in patient populations over the age of 60.
As a surgeon, Dr. Lee became interested in this research after seeing many patients for whom surgery to remove a tumor or to receive a transplant is not a viable treatment option due to the patient’s health or the tumor’s location or size. He was intrigued by the potential to discover treatment modalities. Transplants will never be a viable, sustainable option for addressing the growing prevalence.
“Liver cancer is often not as responsive to chemotherapy and radiation,” Dr. Lee said. “I became interested in figuring out how we can treat these patients with other modalities.”
Destroying Cells Using Light
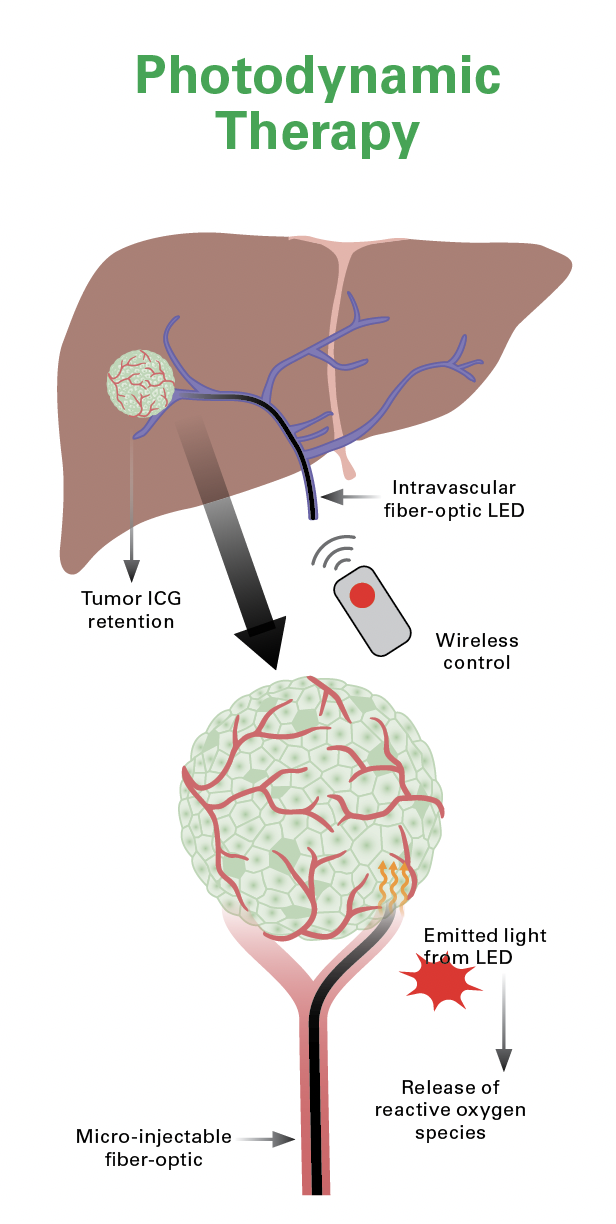
Dr. Lee is exploring how to leverage photodynamic therapy (PDT) to treat this type of liver cancer. PDT is a treatment modality in which clinicians deploy light-sensitive medicines — called photosensitizers or photosensitizing agents — and use a light source to selectively destroy abnormal cells in the affected area.
Dr. Lee’s work has examined how to use indocyanine green (ICG), a fluorescent dye used in medical diagnostics, as the photosensitizing agent.
Liver cancer is often not as responsive to chemotherapy and radiation. I became interested in figuring out how we can treat these patients with other modalities.
Seung Duk Lee, M.D., Ph.D., associate surgical director of liver transplants for the VCU Health Hume-Lee Transplant Center
Once the ICG photosensitizer has been administered, cancer cells are exposed to a specific wavelength of light that causes the photosensitizer to produce a form of oxygen. This begins apoptosis, a type of cell death in which a series of molecular steps in a cell lead to its death.
The process creates a slow, controlled cell death that is noninvasive and differs from similar photodynamic therapies that burn cells and initiate necrosis, a passive and uncontrollable cell death process. This part is key. Being able to administer this treatment to patients who may be sicker will depend on it causing no additional harm.
“We have completed research in animal models given ICG and laser therapy and saw significant reduction in tumor growth,” said Kush Savsani, a first-year medical student. “Currently, we do this with healthy and cancerous models to measure the effect of the photodynamic therapy on the tissue.”
Savsani has been working as Dr. Lee’s research assistant on the project. One of 12 inaugural McGlothlin Scholars at the VCU School of Medicine, Savsani said he chose VCU in part because of the opportunities to engage in this cutting-edge research.
“VCU is unique,” Savsani said. “We have research staff and clinical staff working hand in hand. Because of that, we’re able to do advanced research that maybe other centers aren’t able to.”
Dr. Lee and Savsani are working to advance this potential treatment through continued research. The biggest challenge they’re working to address is how to deliver the necessary light source to tumors in the liver. Their goal is to do so in the most noninvasive manner through use of fiber-optic cabling to deliver the light source via an artery to the affected portions of a patient’s liver.
In 2024, they received commercialization fund assistance from VCU TechTransfer and Ventures, which supports inventors doing innovative research with a clear pathway to take solutions to market by helping them secure patent protections for their work.
“Initiatives like this one embody the intersection of pioneering science and entrepreneurial vision, promising to revolutionize health care,” said P. Srirama Rao, Ph.D., VCU’s vice president for research and innovation. “Through our commitment to fostering innovation and collaboration, VCU continues to lead the way in advancing health care solutions that positively impact lives far beyond our campus.”
What’s Next?
Dr. Lee and Savsani anticipate that the research to demonstrate efficacy and safety will take several years. One benefit of their approach is that the team is using a novel application of existing, approved U.S. Food and Drug Administration devices and treatments as they develop this new modality.
“Using FDA-approved devices helps ease the barriers that similar treatments face when being developed for potential use,” Dr. Lee said. “Once we prove efficacy and safety of these modalities, we can quickly progress to testing the therapy in clinical trials.”
The next step for their research is scaling to models that can offer the testing environment needed to approximate the delivery of the light source via arterial cabling. The team is also interested in exploring a combination of liver tumor reduction through photodynamic therapy and using doxorubicin, a chemotherapy drug commonly used in interventional radiology, through transarterial chemoembolization (TACE). TACE combines delivery of the chemo drug with an embolization procedure when treating hepatocellular carcinoma, and they hope the one-two punch of both therapies may translate to even stronger results for future patients.
“Liver cancer is not a problem we will solve through only organ transplants or surgery,” said Dr. Lee, a robotics transplant surgeon. “What I hope this work can do is to provide a promising treatment option that reduces the burden of cancer and gives hope to future patients.”
If you would like to support this research at the VCU Health Hume-Lee Transplant Center, please contact Andrew Hartley, senior director of development in the VCU Office of Medical Philanthropy and Alumni Relations, at 804-628-5312, or aphartle@vcu.edu.
Support Liver Therapy
Give to the the Hume-Lee Transplant Center.