This Machine was Made for Walking
Article by Tim Shea, VCU Medical Philanthropy and Alumni Relations
Photos by Daniel Min, MCV Foundation
Video by Tyler Trumbo, MCV Foundation
To support research and care for movement disorders, please give now.

Anyone who knows Bill Hicks of Gloucester, Virginia, will tell you the same thing: he’s always on the go. A devoted family man and avid outdoorsman who worked in hospital maintenance for 35 years, Bill rarely had the time or desire to sit still.
I’m just one of these people who really likes to get out and do things.
Whether he was walking miles through the forest to a coveted hunting spot, climbing a ladder to repair wiring at the hospital or teaching his children – and now grandchildren – to appreciate the outdoors, Bill has always led an active, mobile lifestyle.

Smoldering for years
Then he started to notice small amounts of weakness in his legs that later became stiffness – common symptoms that developed slowly and weren’t cause for immediate alarm. However, in 2014, the balance, strength and stamina he’d always known began to diminish. The pain in his legs increased, and walking became a difficult, and dangerous, activity.
Fortunately, after seeing a general neurologist who quickly determined that he required specialized care, Bill was referred to the VCU Parkinson’s and Movement Disorders Center, where he met Leslie Cloud, M.D.
The PMDC’s experts specialize in movement disorders, and Cloud says that the team’s multidisciplinary approach to patient care is one of the center’s strengths. A critical component of Bill’s care was connecting him with the PMDC’s genetic counselors, who discovered that he had a rare disease that only impacts 1 to 10 out of every 100,000 people, or less than 0.01%.
Called hereditary spastic paraplegia, or HSP, the genetic condition causes rigidity in the leg muscles, which greatly impairs a person’s ability to walk.

“The symptoms Bill came to us experiencing had been smoldering for years, and he just wanted to understand what was wrong,” says Cloud, who directs the PMDC’s Parkinson’s disease program. “To have found an answer for him and his family, and a specific one that validated everything they had been through, that phone call was a meaningful moment for everyone.”
With a diagnosis in place, Cloud and the team sprang into action. Step one: Manage Bill’s physical pain. Step two: Keep him as mobile as possible for as long as possible.
To address his pain, colleagues from the Department of Physical Medicine and Rehabilitation outfitted Bill with a baclofen pump, a surgically-placed device that delivers medication to the spine and decreases leg stiffness.
Identifying an appropriate exercise regimen required some out-of-the-box thinking, but Bill’s physical therapists at the PMDC were able to get him the support that he needed, literally.
A motorized ‘dose of exercise’
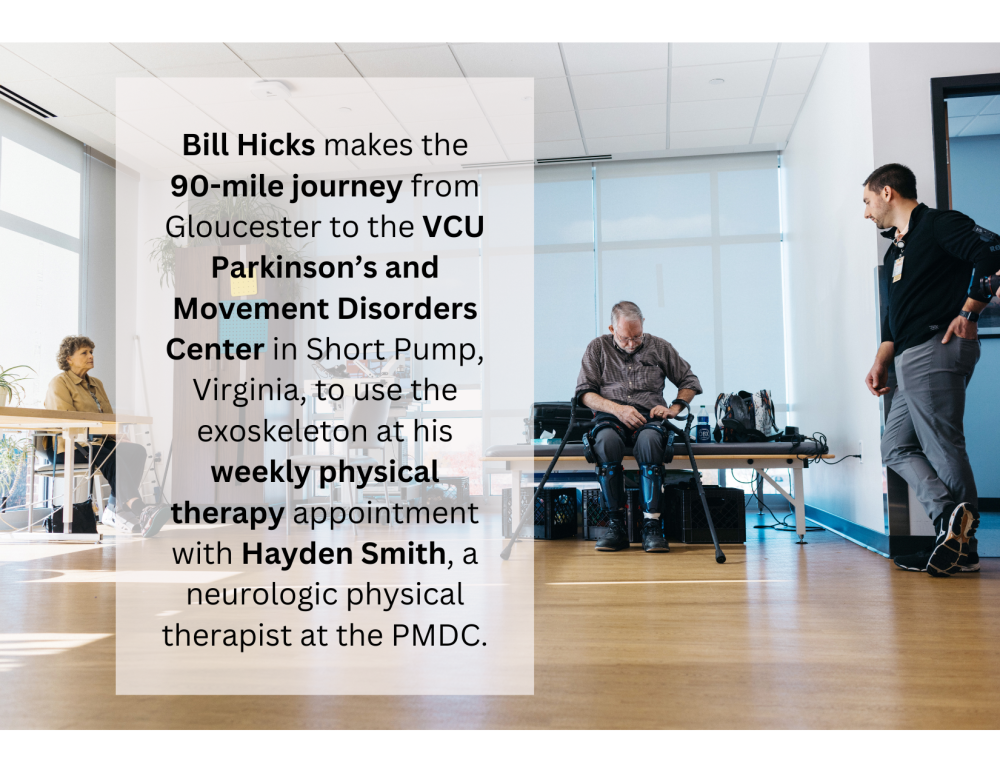
 An exoskeleton is a wearable assistive frame that physical therapists can use to help patients who are living with and recovering from a variety of conditions and injuries. In this case, it’s a motorized frame that stretches from Bill’s hips to his shins and helps him walk independently during his therapy sessions.
An exoskeleton is a wearable assistive frame that physical therapists can use to help patients who are living with and recovering from a variety of conditions and injuries. In this case, it’s a motorized frame that stretches from Bill’s hips to his shins and helps him walk independently during his therapy sessions.
Hayden Smith, a neurologic physical therapist at the PMDC, says the exoskeleton enables Bill to get a higher “dose of exercise” than he would be able to without it.
“The robot is helping him take longer steps, pick his feet up higher and move through a bigger range of motion than the HSP would allow him otherwise,” says Smith, who earned his doctorate in physical therapy from the VCU College of Health Professions. “He’s sustained an amazing walking distance over a period of time, and it’s far beyond what we’d expect with this disease.”
Today, Bill makes the 90-mile journey from Gloucester to the PMDC in Short Pump, Virginia, to use the exoskeleton at his weekly physical therapy appointment with Smith.
“It makes my legs do things that I can’t normally do, and I think it’s the reason that I’m not in a wheelchair,” Bill says.
The exoskeleton has enabled him to maintain the strength needed to continue doing the things he loves. With the support of a pair of canes, he's free to introduce his young granddaughters to hunting and exploring the forest.
Cloud says increasing the number of exoskeletons available for use at the PMDC could benefit more patients living with a variety of conditions such as Parkinson’s disease and amyotrophic lateral sclerosis, or ALS.
The gift of time
Cloud holds the Rogliano Family Endowed Chair at the PMDC. Established in 2019, the position was designed to recruit a clinician-scientist who could help improve outcomes for the patients and families living with Parkinson’s disease and other related movement disorders.
“Time is our most precious commodity, and the chair that the Roglianos generously funded allows me to see patients and devote a portion of my time to pursuing research and developing educational and community wellness programs centered around exercise for this population,” Cloud says.

Both Cloud and Smith admire Bill’s determination and grace in dealing with his diagnosis, and note how rewarding it feels to help him continue to live a full, and fulfilling, life.
Today, Bill is still able to spend time in the same woods he’s been exploring and hunting his entire life.
“Here we go,” he says, zipping up his coat and entering his favorite stand of forest with his two energetic granddaughters by his side. “This is what it’s all about.”

If you would like to learn about opportunities and ways to support neurosciences at VCU Health, contact Allie Betts, director of development, at bettsa@vcu.edu.
Help Others Like Bill
You can support the science and care that went into giving Bill more active time with his family.