Sound Therapy: Using Focused Ultrasound for Essential Tremor
By Holly Prestidge, MCV Foundation
The gold standard for an established decades-old procedure that treats essential tremor faces competition from new technology and advancements that could upend the treatment of tremor-related conditions.
 For the first time, last September, VCU Health performed a procedure called focused ultrasound to treat essential tremor, a neurological condition that causes one’s hands, arms, head, legs or even their core to tremble uncontrollably. Tremors affect more than 10 million people and are about eight times more common than Parkinson’s disease, a similar but different neurological disorder that affects movement and balance.
For the first time, last September, VCU Health performed a procedure called focused ultrasound to treat essential tremor, a neurological condition that causes one’s hands, arms, head, legs or even their core to tremble uncontrollably. Tremors affect more than 10 million people and are about eight times more common than Parkinson’s disease, a similar but different neurological disorder that affects movement and balance.
Where Parkinson’s tremors are typically felt at rest and do not affect the voice box and speech, essential tremor causes shaking when an individual moves and can affect someone’s ability to talk. Essential tremor worsens as people age. Minimal shaking might be annoying, but as the condition progresses, individuals lose their ability to function normally. Researchers and physicians do not know why tremors occur, but they do know how to reduce their severity to allow patients to lead fulfilling lives.
Paul Koch, M.D., a neurosurgeon and director of VCU Health’s focused ultrasound program, led the health system’s first procedure in September 2023 and has performed several since. Focused ultrasound creates a hole, or lesion, in a particular circuit in the brain that effectively disrupts the tremors’ communication pathway.
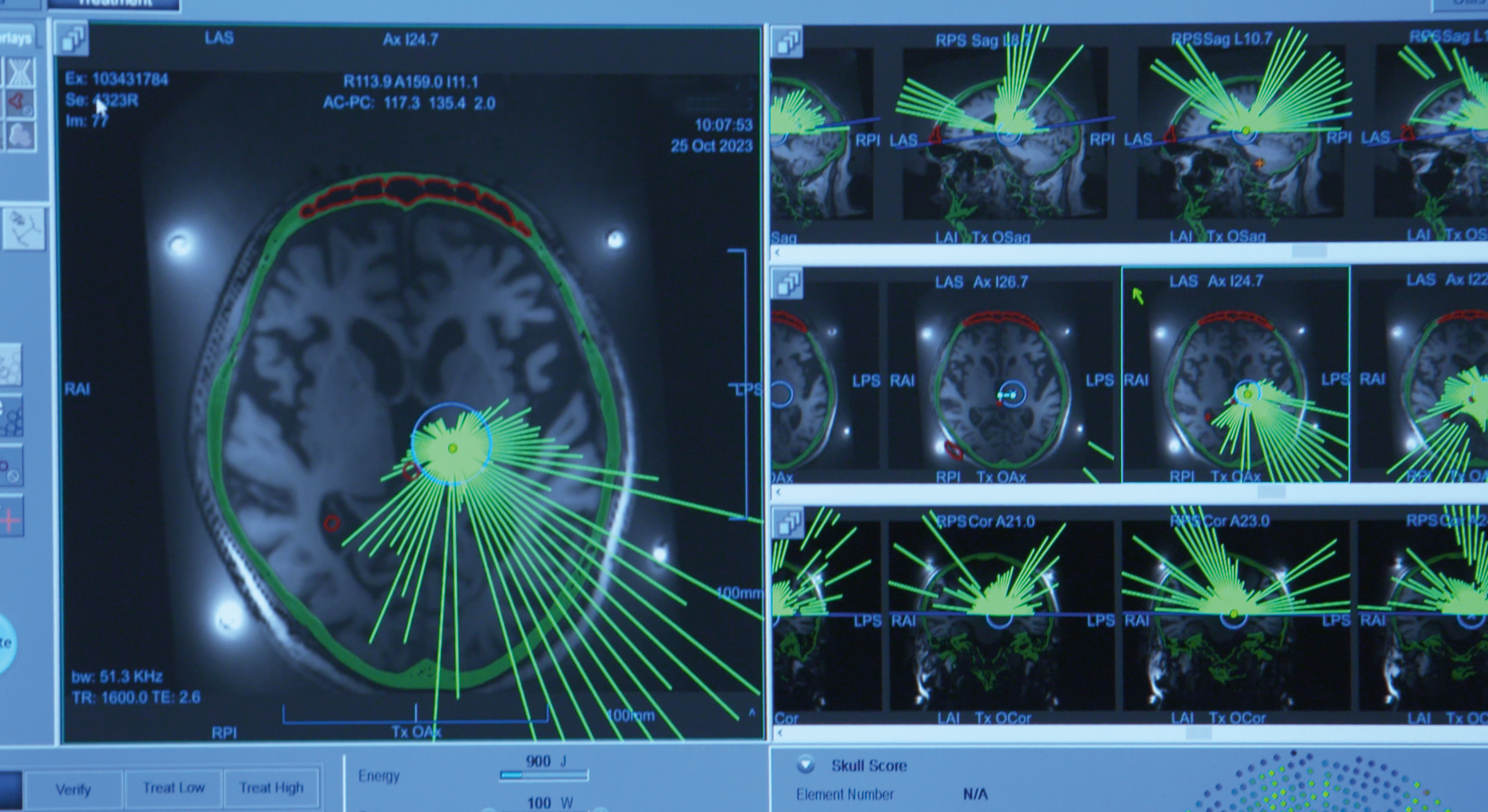
That lesion is created by small bursts of ultrasonic energy pinpointed to an exact location while the patient lies in an MRI machine.
“It was discovered that you could disrupt the tremor, either by putting a hole in the nodes in that circuit or stopping the transmission of communications by delivering electrical stimulation,” Dr. Koch said.
Each burst, called sonication, lasts about 10 to 12 seconds. The first one has the lowest amount of energy — like a test shot — followed by increased energy in subsequent bursts. Between each burst, patients are checked for potential side effects like slurred speech or tingling and numbness in their hands or other parts of their body.
As the procedure moves forward, patients and physicians detect whether tremors have already lessened by working through tasks that test fine motor skills. Patients typically receive about six to 10 bursts during the entire outpatient procedure, which only takes a matter of hours and for which general anesthesia is not necessary.
Relief can be felt very quickly.
“The most critical thing is, are the tremors significantly impacting their lives,” Dr. Koch said. “It’s all about improving people’s functionality and quality of life.”

New Technology for an Established Procedure
For years, patients with tremors had been treated using deep brain stimulation, where electrodes are surgically implanted into the brain and act as a sort of switch that disrupts the tremors with electrical stimulation.
VCU Health has been a leader in deep brain stimulation for decades, thanks largely to Kathryn Holloway, M.D., a neurosurgeon and director of the deep brain stimulation program. Dr. Holloway has completed hundreds of DBS procedures, and she was part of a team that developed and researched frameless DBS technology.
Dr. Koch explained that both DBS and focused ultrasound disrupt the same circuitry in the brain, but there are differences between the two, and in some cases, focused ultrasound offers benefits both now and in the future. To start, DBS requires general anesthesia, which is high risk for some people. And patients who are on blood thinners are required to go off those medications for roughly two weeks before surgery, which could be risky for them.
Risks are inherent with any surgery, and for those undergoing DBS, the highest risks come during the procedure, from bleeding and infections. Following surgery, the electrodes are permanent, and need to be monitored and maintained regularly throughout the patients’ lives, to address their condition.
Focused ultrasound does not require permanent electrodes or general anesthesia. Similar to DBS, the procedure uses a localized anesthetic on the scalp when patients are fitted into a stabilizing apparatus before using MRI scans to map the brain and identify treatment targets. During this phase, patients in both procedures remain awake and alert, but DBS requires a second surgery under general anesthesia to implant a pulse generator in the chest wall that is connected subcutaneously to the permanently implanted electrodes.
Once doctors determine where the lesion will occur, they begin with several low-energy sonications to make sure the location is exact. If it is not, the target can be moved without any negative impact.
Unlike deep brain stimulation, the risks of focused ultrasound tend to be longer term, such as challenges with gait or lingering tingling and numbness in hands or mouth. While patients may experience those side effects for days or a few weeks, 90% of patients recover.
“Focused ultrasound is a new technology to do an old procedure, and it’s more precise, more convenient and safer for the patient,” Dr. Koch said. “For people who take medications and can’t undergo general anesthesia or can’t be in the hospital for days with a traditional surgical setting, this offers a significant advantage.”
Dr. Koch explained that the FDA has approved focused ultrasound to treat essential tremor as well as tremor-dominant Parkinson’s disease. It has also been approved to treat both sides of the brain, though both sides can’t be treated at the same time as surgeons need to determine if there are side effects after the initial procedure. If patients require a second procedure, the FDA requires a minimum wait time of nine months.
 The data thus far, said Dr. Koch, shows that focused ultrasound can help ease essential tremor for about five years, though that varies by patient, as the treatment addresses only the symptoms of an underlying condition that will never go away.
The data thus far, said Dr. Koch, shows that focused ultrasound can help ease essential tremor for about five years, though that varies by patient, as the treatment addresses only the symptoms of an underlying condition that will never go away.
Focused ultrasound has been approved for essential tremors in people ages 22 and older, while DBS is available for people ages 30 and up. Dr. Koch said the future of focused ultrasound includes treating patients not only with essential tremor and tremor-dominant Parkinson’s, but also individuals with epilepsy.
While current clinical focused ultrasound uses high-frequency energy, low-frequency therapies are being studied as a means of temporarily opening what doctors call the blood-brain barrier.
The brain is a specialized compartment, and not everything that travels through the blood can easily get into the brain. This is a good thing when it comes to infections and toxins. However, it also means high concentrations of drugs such as chemotherapy are needed to get through that barrier, which can cause negative side effects in the body.
Low-frequency focused ultrasound could potentially open that barrier just enough in just the right place and for enough time that drugs are able to get through to targeted specific locations. Those abilities could change the landscape for chemotherapy or immunotherapies as well as gene delivery procedures, Dr. Koch said.
“What we do now with focused ultrasound is just the tip of the iceberg,” he said. “This is a promising technology, both for high- and low-frequency focused ultrasound, and it’s really positioning VCU Health to take the next steps in delivering truly personalized medicine.”
If you would like to learn about opportunities and ways to support neurosciences at VCU Health, please contact Allie Betts, director of development for neurosciences and psychiatry in VCU’s Office of Medical Philanthropy and Alumni Relations, at 804-828-3407 or bettsa@vcu.edu.
Discover More
Read more features like this in the summer issue of NEXT magazine.
